Congratulations to our Poster Award Winners
1st Place - Potential herb-chemotherapy or radiation interactions in patients with cancer: A prospective study of the pharmacist and student-pharmacist run herbal assessment service at the University of Vermont (UVM) Cancer Center - J. Schwartz, A. Tran
2nd Place - Incidence of Potential Germline Mutations in Cancer Patients with Genomic Testing - P. Sharma, H. Wright, M. Sands, E. Folefac, M. Wood
3rd Place - Enhancing Bone Marrow Transplant Care through the Patient Experience - A.Prokopik, L. Wesinger, C. Morton, J. Holl, J. Gentes, S. Rossi, S. Smith, A. Riley, S. Aldrich, M. Bennett, J. Coffey, J. Hill, Jr.
4th Place - Cancer patients with self-identified food insecurity report a higher symptom burden than food secure patients - E. Longnecker, T. Weisberg, C. Thomas,
5th Place - TIE -
- Targeting CLL and MCL cells with DNA repair and B cell receptor inhibitors - L. Shopland, A. Curtis, A. Moineau, D. Pham, S. Rajan, R. Zhang, E. Brooks, T. Hoffert, J. Rueter
- Acute Heart Failure due to Autoimmune Myocarditis from Pembrolizumab - S. Waldstein, S. Kodali, M. Barry
Accepted Abstracts
Thrombin Generation as a Predictive Biomarker for Venous Thromboembolism in Patients with Pancreatic and Lung Cancer Undergoing Systemic Therapy
A. Ajala, M. Cho, L. Salvatore, D. Ornstein, M. Drescher
Dartmouth Hitchcock Medical Center
Background: The Khorana score (KS) predicts the risk for chemotherapy-associated VTE, but is assessed only at one time prior to treatment. The aim of our study was to determine if assessment of TG (both peak TG and endogenous thrombin potential (ETP)) improves VTE risk prediction compared to the KS alone and to evaluate the impact of systemic therapy on TG over time.
Methods: We enrolled 15 adults with newly diagnosed lung or pancreatic cancer. KS was calculated once. TG blood samples were obtained at the beginning of each of the three chemotherapy cycles.
Results: TG were 341, 324, 641 and 890 nmole, and mean ETP were 1459, 1685, 2155, 2051 nmole/min for KS 1,2,3 and 4, respectively. Both peak TG and ETP decreased over time after cancer therapy. VTE occurred 27%, and the median KS was 2 for patients with and without VTE. Mean peak TG was similar in patients with and without VTE but mean ETP was higher in patients with VTE.
Conclusions: Preliminary results suggest that there is a direct correlation between KS and peak TG and ETP, and that ETP may be a more reliable predictor VTE than KS in cancer patients. Peak TG and ETP decreased after initiation of systemic therapy, suggesting that the degree of coagulation activation is proportional to tumor burden. These data suggest that TG is a promising biomarker of VTE risk.
Food Insecurity at New England Cancer Specialists: An Exploratory Study
R. Ali, T. Weisberg
University of Southern Maine, New England Cancer Specialists
Background: Food insecurity is a state of being without reliable access to a sufficient quantity of affordable and nutritious food. In this study we identified the prevalence of food insecurity among patients at New England Cancer Specialists. An observational hypothesis prior to data collection was that an underinsured state would correlate with more food insecurity.
Methods: Over 6 months, 5135 patients were screened for food insecurity using a validated 3-item screening tool. We performed descriptive statistics to examine patients’ demographics, health insurance status, cancer diagnosis, and therapy.
Results: 104 patients screened positive for food insecurity. 61% women and 39% men. Age of patients ranged from 18 to 80+ years with the highest percentage of patients being age 50-59. 94% of food insecure patients had a primary care physician. 97% had healthcare insurance (Mainecare 17%, Medicare with supplemental 39%, Medicare only 6%, and private insurance 34%) with only 3% uninsured. Patients with a solid tumor diagnosis comprised 72% of patients, Leukemia/Lymphoma 12%, benign hematology and other disorders 15%. Patients experienced treatments ranging from observation to combined modality therapy.
Conclusions: Food insecure patients were more likely insured than uninsured. One third of patients had private insurance. Food insecurity was not always associated with aggressive cancers and cancer therapies but was identified in individuals with benign hematology diagnoses. We plan to explore these associations in future studies and attempt to link food insecurity to cancer treatment outcomes.
The Maine Cancer Genomics Initiative (MCGI): Launching a Community Genomic Medicine Program in Community Practice in Maine
A. Antov1, P. Helbig1, J. Bourne1, R. Male1, H. Reddi1, S. Mockus1, K. Adams1, K. Reed1, E. Edelman1, L. Waterston2, S. Miesfeldt2,P. Han2, J. Rueter1
1The Jackson Laboratory, 2Center for Outcomes Research and Evaluation (CORE) at Maine Medical Center Research Institute
Background: Sophisticated NGS-based genomic tests interrogating a large number of genetic alterations in tumor tissue have recently been developed but many barriers exist in the integration of these methodologies into community practice. The MCGI, a partnership between JAX and the largely rural Maine oncology community, was established to facilitate the integration of novel genomic technologies into community oncology practice.
Methods: MCGI goals are enabled by network and governance creation, the provision of educational opportunities to clinicians and genomic tumor board support as well as the conduct of a prospective, multi-site study protocol investigating clinician and patient experience with clinical genomic tumor testing.
Results: The MCGI Forum, an initial meeting of clinicians and research staff from the Maine oncology community, was held in Feb 2017. It was attended by 23 clinicians and 27 research and administrative staff from 16 practices. In May 2017, the Study protocol received IRB approval, allowing sites and clinicians to enroll. To date, 3 practices have enrolled as sites and 1 practice will refer patients to the central site at the MCGI office for study participation. Subjects participating to date include 16 clinicians and 7 cancer patients. The initial educational module and MCGI-supported genomic tumor boards have been launched.
Conclusions: The Maine Cancer Genomics Initiative is an opportunity for both translational implementation and research by the Maine oncology community. Onboarding and enrollment of sites and clinicians on the study has proceeded swiftly, indicating the potential for additional translational outreach opportunities in other healthcare systems and geographic areas.
Precision Medicine: The challenges and successes of molecular profiling at Dartmouth-Hitchcock Medical Center
M. Chamberlin1, Erica Bernhardt1, A. Ajala1, D. Findley2, G. Tsongalis2, I. Gorlov2, T. Miller2, L. Tafe2
Dartmouth Hitchcock Medical Center1; Geisel School of Medicine at Dartmouth2
Background: Dartmouth has been performing next generation sequencing (NGS) on tumor specimens since 2013. The Molecular Tumor Board (MTB) was formed in 2013 to assist clinicians in interpreting the results and identifying potential treatments. Clinical triais are increasingly requiring mutation information. We describe the evolution of our molecular oncology program since 2014 and the efficacy of different data collection methods.
Methods: Data from our clinical trial, MTB, EMR and molecular pathology databases were reviewed between 2014 and 2017. A searchable molecular tumor board note was created to extract data from the electronic medical record and compare to manually entered data
Results:
Conclusions: Molecular profiling is increasingly required for clinical trial enrollment however less than 10% of patients are enrolling on molecularly based trials and less than 5% are presented at a Molecular Tumor Board. A data extraction tool did not capture clinical data reliably. Improvements in data collection systems are essential to evaluate the outcomes of multi-disciplinary programs. A quality improvement project is underway.
cole poster.pdf
Use of a validated survey instrument to assess functional outcomes of rectal cancer treatment in a community hospital setting
K. Cole1, K. Lehmann1, D. DiCesare2
1Portland Surgical Associates, 2 Tufts University School of Medicine
Background: Patients undergoing rectal cancer treatment may develop bowel, urinary, and sexual functional difficulties weeks to months after treatment; screening for these issues can be challenging in the absence of a centralized, multi-disciplinary clinic. We used a validated survey tool to help identify these patients.
Methods: Surveys were offered postoperatively to all patients undergoing rectal resection with pelvic dissection between February 2012 and July 2017. The survey was modified from the EORTC (QLQ-CR29) validated questionnaire. A response of 3 (“quite a bit”) or more on any survey item prompted consideration for intervention
Results: During the study period, 32 patients were surveyed. 21 patients returned at least one survey (66%); 29 out of 51 total surveys (57%) were returned. 12 of the 29 surveys (41%) were completed during a follow-up visit, while 17 (59%) were returned by mail. During the study period, 9 out of 21 patients (43%) assigned a score of ≥3 at least once for a bowel function item; 4 out of 21 patients (19%) for a urinary function item; and 7 out of 21 (33%) for a sexual function item. A total of 12 out of 21 patients to return a survey (57%) were offered interventions and 5 out of 12 accepted (42%)
Conclusions: Use of an existing survey instrument allowed us to identify and treat patients with functional problems related to rectal cancer treatment independent of scheduled follow-up, improving the quality of survivorship care in our community hospital.
Relapse of follicular lymphoma: a bevy of buttock cells
C. Del Prete, J. H. Feng, F. Lansigan, E. Bengtson, R. Kubica
Dartmouth-Hitchcock Medical Center
Background: Follicular lymphoma (FL) is considered an indolent non-Hodgkin lymphoma, rarely associated with a leukemic phase. We report a 58-year-old male with history of FL, diagnosed two years prior with extensive adenopathy and treated with bendamustine and rituximab. Therapy was discontinued after two cycles due to intolerance. He achieved partial remission and was followed prospectively. He presented with debilitating lower extremity swelling. Dopplers were negative for DVT though extensive pelvic adenopathy was detected. Labs showed a critical white count and tumor lysis. He was admitted to the hematology service.
Methods: Case report
Results: Labs revealed WBC 463K (9K two months previously), Hgb 7.3, Plt 63K and LDH 740 (110-220 u/L). The differential diagnosis at this time included histologic transformation to more aggressive lymphoma such as diffuse large B-cell vs CLL/SLL. A peripheral smear revealed leukocytosis with 91% atypical lymphocytes, described as “buttock cells”, consistent with leukemic phase of FL. Flow cytometry demonstrated a monoclonal lambda-restricted CD10+ CD20+ B-cell population. A PET-CT showed extensive FDG avid bulky adenopathy in the neck, chest, abdomen, and pelvis along with massive splenomegaly. A lymph node biopsy revealed FL with Ki67 of 10-20% and a bone marrow biopsy showed 95% involvement with FL. The patient was treated with COPE (cyclophosphamide, vincristine, prednisone, and etoposide) and rituximab was added once WBC<50K. Therapy is ongoing with dramatic response to date.
Conclusions: Our patient was admitted with suspicion of transformation to high grade lymphoma; however, subsequent work-up revealed leukemic phase of follicular lymphoma, a rarely reported entity associated with a poor prognosis.
Is Brain MRI necessary in the pretreatment evaluation of early stage NSCLC?
C. Del Prete, G. Wasp, J. Farrell, K. Dragnev, G. Russo, G. Atkins, G. Brooks
Dartmouth-Hitchcock Medical Center
Background: At present, there is limited evidence and conflicting guidelines on when to include brain MRI in the pretreatment evaluation of NSCLC.
Methods: We retrospectively reviewed data from eligible patients who underwent work-up for newly diagnosed NSCLC from January 1 to December 31, 2015. We identified all records of pretreatment neuroimaging within 12 weeks of diagnosis, inclusive of CT head (CR) or brain MRI (MRI). The indication for neuroimaging, presence of neurologic symptoms, cancer stage (excluding neuroimaging), and the presence of brain metastases were abstracted.
Results: 157 of 216 patients (72.7%) underwent neuroimaging (144 MRIs, 13 CTs). Only 41 patients (26%) underwent imaging for neurologic symptoms while the remainder were asymptomatic (74%). Of those, 28 (68%) were found to have a brain metastasis. Among asymptomatic patients, 19 were stage I and 16 were stage II prior to neuroimaging. No brain metastases were discovered. For more advanced NSCLC (also asymptomatic), 37 patients had stage III and 44 stage IV disease: brain metastases were found in 4 (11%) and 9 (20%) patients respectively.
Conclusions: In patients with early stage NSCLC (stage I and II) without neurologic symptoms, neuroimaging did not reveal any brain metastases. Continued use of neuroimaging in the pretreatment evaluation of clinical stage I-II NSCLC may be unwarranted.
H3 K27M-mutated gliomas in adults: is there a potential role for immunotherapy?
V. Forbes, S. Coker, P. Rauschkolb
Dartmouth-Hitchcock Medical Center
Background: Diffuse H3 K27M-mutant gliomas are rare in adults and carry a dismal prognosis. They appear histologically low-grade, but are considered WHO grade IV regardless of their microscopic features. After surgical resection and radiotherapy, the optimal adjuvant treatment regimen remains unknown.
Methods: We describe an adult patient with a midline H3 K27M-mutated glioma treated with immunotherapy.
Results: Our patient is a 43-year-old gentleman who presented with headache, visual distortion, and imbalance. He was found to have a thalamic mass. Biopsy was suspicions for an infiltrating glioma, with atypical glial cells staining positive for H3 K27M. He underwent radiation with concurrent temozolomide followed by adjuvant temozolamide. He required a treatment break due to intolerance, but exhibited radiographic stability. Surveillance MRI revealed progression in the form of new intraventricular lesions. He experienced a rapid decline physiologically and was treated with bevacizumab over surgery. When he progressed, he was switched to pembrolizumab. Further progression beckoned an alternate plan to be devised including pembrolizumab followed by radiotherapy then pembrolizumab. His repeat MRI was concerning for progression despite the propensity for immunotherapy to increase the volume of enhancement. After a difficult discussion, he declined further treatment and transitioned to hospice care.
Conclusions: Diffuse H3 K27M-mutant gliomas are aggressive tumors for which no optimal treatment has been identified. Further investigation of the role of immunotherapy in treating these challenging tumors is paramount.
Dual-Tandem Brachytherapy for Stage I Endometrial Cancer
H. Gagne1, D. Arsanious2, T. Ashikaga2
1UVMMC Department of Radiation Oncology; 2University of Vermont Larner College of Medicine
Background: Outcome data on toxicities from dual-tandem brachytherapy for patients with medically inoperable endometrial carcinoma is scarce. The purpose of this report is to describe technique and toxicity in this population.
Methods: Patients with stage I endometrial cancer treated non-operatively between 2008 and 2016 with dual-tandem brachytherapy were reviewed. Demographic, disease-specific, treatment, and toxicity data were collected. Two-sample t-test was used to compare the frequency of gastrointestinal (GI) and urinary toxicities between subgroups.
Results: Twenty-two patients were treated between 2008 and 2016. Median age was 61.5. Median BMI was 50.8. Regarding surgical contraindications, obesity and pulmonary comorbidities were the most commonly encountered, present in 81.8%and 68.2% of the study population, respectively. GI, urinary, and gynecologic toxicities occurred in 36.4%, 36.4%, and 4.5% of patients, respectively. No patient experienced Grade4 or 5 toxicity. Two-sample t-tests demonstrated a significantly lower prevalence of GI toxicities in patients who underwent treatment with filled bladder (p=0.009) and did not receive external beam radiation (p=0.001). Local control was achieved in twenty-one patients (95.5%). Overall survival was 81.8% (18 patients) after a median of 42±25 months (range 1-86 months) in follow-up. Endometrial cancer-specific mortality was identified in one patient (4.5%) and death from inter current disease was identified in 3 patients(13.6%).
Conclusions: Favorable clinical outcomes for patients with stage I endometrial cancer are achievable from dual-tandem brachytherapy. Our data suggest that maintaining a full bladder during treatment appears to significantly lower the frequency of GI toxicities without detriment to the bladder.
Scheduling to ALL Infusion Limits
M. Howe, M. Brown, G. Brooks, A. Chadwick, D. Crosby, D. Gelb, J. Hickman, E. McGrath
Dartmouth Hitchcock Medical Center
Background: Infusion scheduling was guided by two capacities: chair space, and pharmacy dose preparation. Frequently, one or more of these capacities was reached, hindering ability to appropriately schedule additional patients. This caused increased patient wait times; secretary and provider frustration; and leadership fielding increased exception requests. Hourly nursing capacity was not considered, resulting in patient care delays and nursing overload.
The goals of this work were to understand overall infusion capacity, identify existing opportunity, optimize all resources, and improve patient experience.
Methods: The team used the DMAIC method for process improvement. Time and motion study data was used to understand nursing workflow and capacity. The team measured capability per hour per day for each of the three capacities and identified opportunities for additional appointments between 8am and 11am.
Results: Several pilots were run focusing on increasing the number of patients scheduled in the morning. Newly understood nursing capacity was integrated with pharmacy and chair capacities. Timeliness and nurse workload were monitored during each pilot.
Conclusions: New scheduling guidelines that take into account chair space, pharmacy dose capacity, and nursing workload were implemented. Sustained improvement results include 84% of patients receiving on-time treatment (increased from 77%) and 89% of patients ending their treatments on time or early (increased from 83%). Staff feedback includes reduced frustration with scheduling patients and more manageable nurse workload.
Pancytopenia and hemolysis
W. Jehangir, E. Umyarova, H. Tul Rehman
University of Vermont Medical Center
Background: Anaplasmosis is most frequently reported from the upper Midwestern and northeastern of US and New York, Connecticut, New Jersey, Rhode Island, Minnesota, and Wisconsin accounts for 90% of all reported cases.
Methods: A 78 years old white male with past medical history significant for prostate
cancer status post prostatectomy, OSA who admitted to the hospital for pancytopenia. His baseline Hb was 15 which dropped to 10.4. His WBC count dropped from 4.06 to 1.57 and platelets dropped to 33 (from 140). Patient was admitted to the hospital with episodes of fever and pancytopenia. His heptoglobin was <6, LDH was 1435 but peripheral smear did not reveal any schistocytes. His coagulation panel revealed prothrombin time 13.9, INR 1.2, PTT 24 and fibrinogen 351. His D-dimer was 912 and direct antiglobulin test was negative. His ultrasound abdomen showed splenomegaly. He underwent an infectious workup that was negative for RSV, metapneumovirus, influenza A & B, parainfluenza, hepatitis B, hepatitis C, parvovirus infection, and thick smear showed no evidence of parasitic infection, but his Anaplasma titers were <1:64, and subsequent PCR for Anaplasma was positive. Patient was started on doxycycline. His most recent counts showed recovery with Hb 13.5, WBCs of 4.39 and platelets of 231.
Results: The number of cases reported to CDC has increased steadily from 348 cases in 2000, to 1761 cases in 2010. This case focuses on the importance of thinking outside the box of hematologic causes of pancytopenia especially with increasing numbers of reported cases.
Conclusions: Patient counts are recovering.
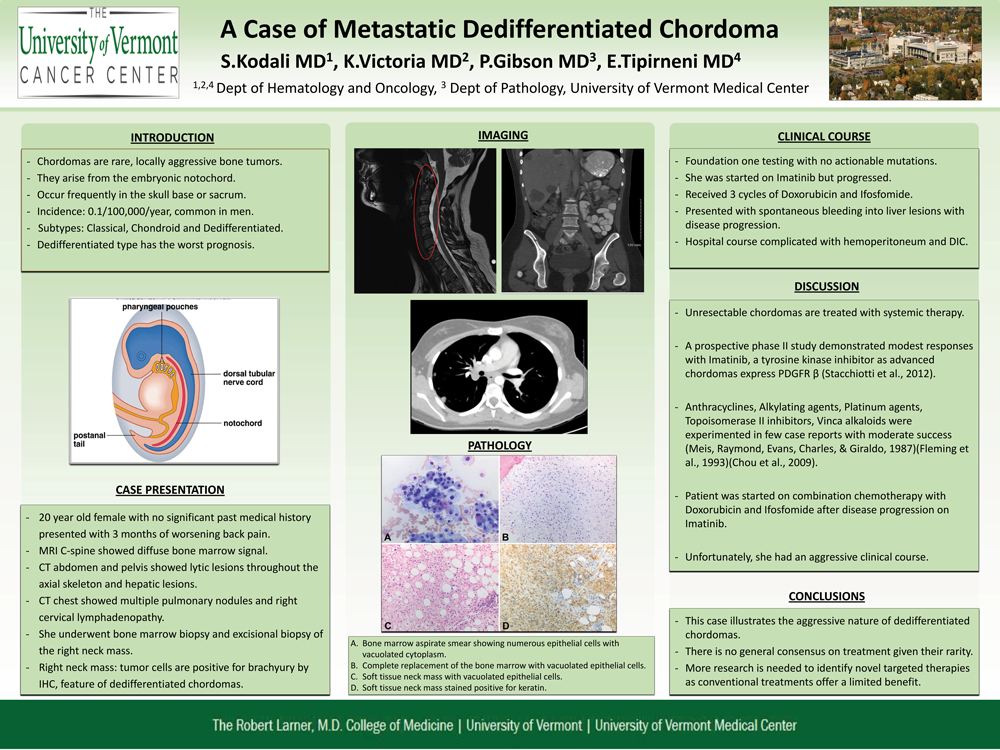
A Case of Metastatic Dedifferentiated Chordoma
S. Kodali, K. Victoria, E. Tipirneni
The University of Vermont Medical Center
Background: Chordomas are rare but locally aggressive bone tumors, which arise from the embryonic notochord. The incidence has been reported to be 0.1 per 100,000/year. They occur most frequently in the skull base or sacrum. They are more common in men. We report a 20-year-old female presenting with metastatic dedifferentiated chordoma.
Methods: A 20-year-old female with no significant past medical history presented with 3 months of worsening back pain. MRI showed T5, S1 pathologic fractures with diffuse bone marrow infiltration. Further staging work-up revealed: multiple lesions in lungs, liver and 2 soft tissue lesions on the scalp.
Results: Bone marrow biopsy showed: solid sheets/nests of cells with vacuolated cytoplasm. IHC was positive for brachyury, which is diagnostic for chordomas, with loss of INI-1, indicating features of dedifferentiation. Foundation-one testing did not show actionable mutations. Imatinib was shown to be active in advanced chordomas but she did not respond. Based on data demonstrating modest responses with anthracyclines and alkylating agents in dedifferentiated chordomas, she was started on doxorubicin and ifosfomide. She had disease progression after 3 cycles and had spontaneous bleeding into one of the liver lesions complicated with hemoperitoneum and DIC. After a protracted hospital course, she was transitioned to comfort measures only.
Conclusions: Chordomas are classified into classical, chondroid and dedifferentiated types. Dedifferentiated chordomas have poor prognosis as depicted by our case. There is no general consensus on treatment given their rarity. More research is needed to identify novel targeted therapies as conventional treatments offer a limited benefit.
Haploidentical Stem-Cell Transplant for Hematologic Malignancies: Rationale and Early Experience from a Single, Rural-Based Transplant Center*
R. Lizcano, D. McKenna, C. Lowrey, C. Hayes, S. Brighton, L. Root, K. Wilcox, E. Busnach, C. Coughenour, K. Meehan, J. Hill, Jr.
Blood and Marrow Transplant Program, Norris Cotton Cancer Center, Dartmouth-Hitchcock Medical Center
Allogeneic stem cell transplantation (SCT) is a potentially curative intervention for many hematologic malignancies. However, a major barrier to its use is limited donor availability, as only one third of patients will have an HLA-matched sibling donor, and matched unrelated donors are often unavailable.
Alternatively, use of HLA-haploidentical (“half HLA-matched”) relatives as donors offers an expanded and readily available donor pool, though this has been limited by intolerable rates of graft-versus-host disease (GVHD), a donor T-cell mediated phenomenon. Most recently, implementation of post-transplant cyclophosphamide (PT-Cy) to suppress donor T-cells after haploidentical SCT has achieved improved GVHD control and therefore overall viability. Based on this advancement, we sought to enhance transplant feasibility at our center by initiating haploidentical SCTs in early 2017.
To date, 4 haploidentical transplants have been undertaken, utilizing Fludarabine/Cyclophosphamide and total body irradiation (Flu/Cy/TBI) conditioning with PT-Cy. All 4 patients engrafted after tolerating pre-transplant conditioning, and 3 of the 4 maintain intact counts. The remaining patient was successfully treated for CMV reactivation with a delayed drop in counts (potentially ganciclovir related) and is now undergoing further work-up. All 4 patients remain in remission, and none have developed clinically evident GVHD. Four additional haploidentical transplants are pending, and we anticipate 10-12 annually.
Haploidentical SCT represents a viable alternative for patients without otherwise suitable donors. The feasibility of receiving this modality safely at our rural-based transplant center will optimize local support of family and reduce the financial and emotional hardships of referral elsewhere, thereby enhancing the transplant experience.
Cancer patients with self-identified food insecurity report a higher symptom burden than food secure patients
E. Longnecker, T. Weisberg, C. Thomas,
New England Cancer Specialists
Background: Introduction: One in eight residents in Maine are food insecure, higher than the national average of one in six. NECS is partnered with a local food bank to help identify food insecure patients so they can receive services. The current study was aimed to understand how food insecurity affects patient reported outcomes (PRO) in a hematology/oncology practice.
Purpose: To determine if food insecurity is associated with a change in symptom burden reported in PRO surveys.
Methods: Between January and July 2017 we identified 86 oncology/hematology patients who indicated food insecurity as part of their PRO survey, distributed prior to each patient visit. Food secure case control matches controlled for disease, stage, gender and age (n=86) were identified during the same time period. The following PROs were assessed and graded based on CTCAE 4.0 guidelines: difficulty sleeping, fatigue, pain, mood and appetite.
Results: Patients indicating food insecurity reported a higher symptom burden compared to case control matches (table 1). Using a correlated t-test, the differences in scores were found to be statistically significant (99% power) for each symptom except appetite (85% power).
Conclusions: Cancer patients with food insecurity self-report a significantly higher burden of symptoms compared to matched controls who are food secure. We hypothesize that improved access to social services could alleviate the symptom burden of cancer patients irrespective of disease related factors.
 Improving Oral chemotherapy adherence
Improving Oral chemotherapy adherence
R. Macpherson, C. Moores
Mercy Hospital
Background: The volume of oral oncolytic continues to increase posing unique clinical and patient safety risks that have challenged oncology care giver to address. Mercy Hospital’s Oncology Program has implemented a consistent process, incorporating current ASCO/ONS Chemotherapy Safety Standards that clinicians follow when initiating treatment with an oral oncolytic. This helps to minimize safety risk and ensures our patients receive the highest level of care. Patients are screened, educated and monitored for adherence and tolerance.
Methods:
Patient Education, in the form of a visit to the office to meet with the multidisciplinary team for formal information on the treatment.
Weekly phone calls utilizing motivational interviewing, regular scheduled follow ups and ongoing patent education and engagement are all strategies used to help with adherence.
All interactions documented in EMR.
An attempt is made to meet face to face with each office visit.
Results: Increased patient adherence and better outcomes, through multidisciplinary education and motivational interviewing and follow up.
Conclusions: Adherence is utmost importance for safe patient care and remains an important focus of oncology clinicians. Non- adherence leads to decrease in efficacy, toxicities due to side effects. It may also increase the number of hospitalizations and ED visits. These would be visits that may have been avoidable and may cause undo financial burden. Adherence can be increased through: education and patient engagement prior to initiation of treatment and ongoing throughout course of care.
Transportation barriers and solutions for Maine cancer patients
P. Madden1, A. Sheikh2, J. Charles1
1 Market Decisions Research; 2 Maine Cancer Foundation
Background: Access to transportation is critical for cancer patients. Research demonstrates that lack of transportation and greater travel distances significantly reduces the likelihood that patients receive first-line oncology treatment and influences the types of treatment they receive. Transportation barriers also disproportionately affect those in rural areas, many of whom lack access to oncology providers.
Methods: A comprehensive cancer transportation needs assessment combined data from multiple sources, including inpatient and outpatient hospital encounters, the Maine Cancer Registry, licensed provider lists and a survey of transportation service providers. GIS mapping was used to visualize where patients travel to receive care. We also examined transportation availability and need by geography, demographics and type of treatment received.
Results: Three counties in Maine have no oncology providers and nine lack radiation treatment services. Those living in isolated rural areas traveled an average of 60 miles to receive treatment, compared to 14 for those in metro areas. Lower socioeconomic status is associated with elevated cancer incidence rates, more transportation barriers and fewer visits for treatment. Three-quarters of transportation providers rely on volunteer drivers and half do not have adequate funding to meet demand.
Conclusions: Solutions to transportation barriers must be tailored to the community. Rural areas of Maine lack access to oncology providers, so innovative solutions are needed to bring services closer to where patients live. Increased public funding for transportation is vital for reducing transportation barriers. Other solutions include community-based transportation providers, implementation of transportation-friendly policy, telemedicine, lodging resources, and volunteer community-based driver networks.
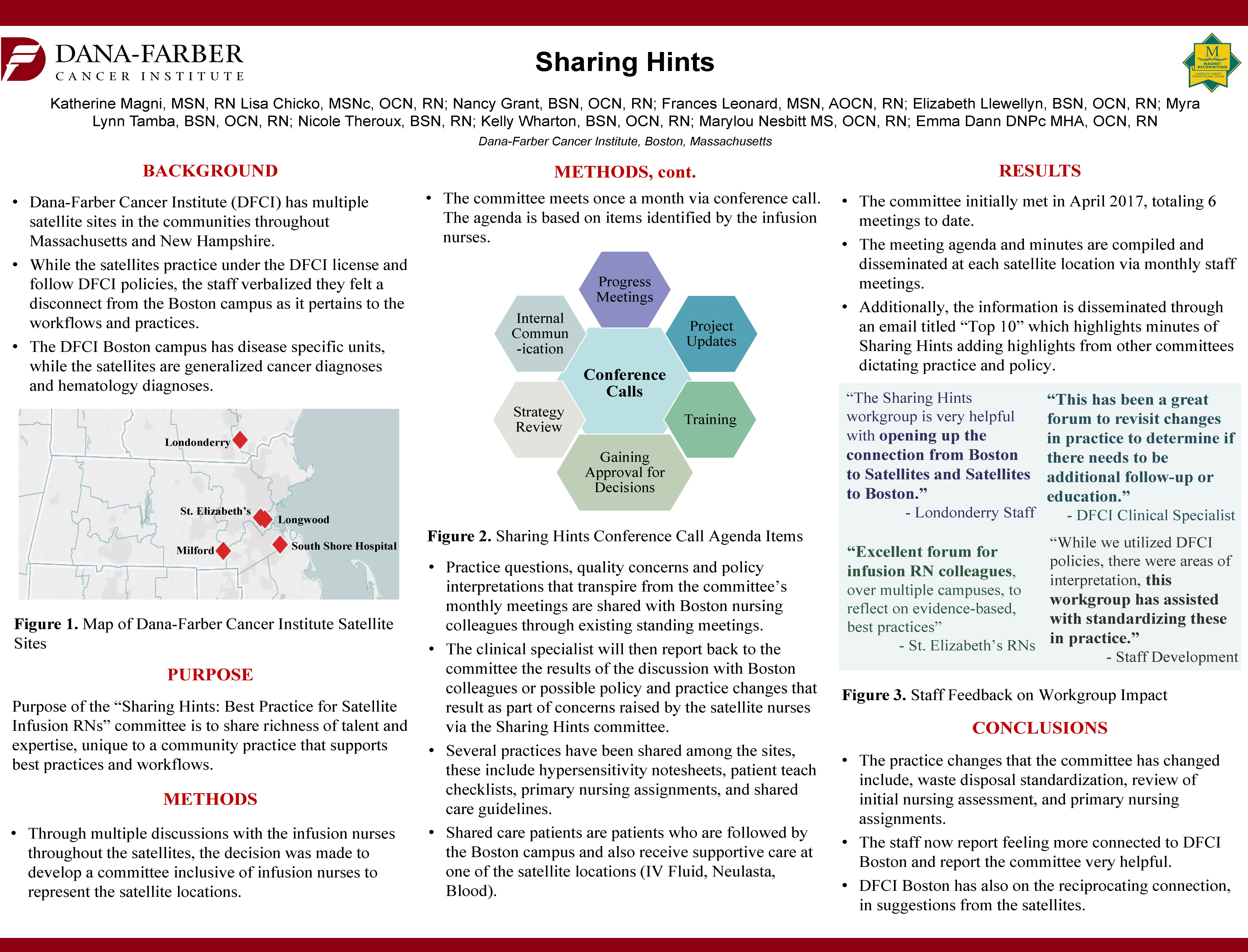
Sharing Hints
K. Magni, Dana Farber Cancer Institute
Background: Dana Farber has multiple satellite sites in communities throughout New England. Satellite staff verbalized they felt a disconnect from the Boston campus as it pertains to the patient population. The Boston campus has disease specific units, while the satellites are generalized oncology and hematology diagnoses.
Methods: Through multiple discussions with infusion nurses throughout the satellites, the decision was made to initiate a committee to represent satellite locations. The multi-site committee meets monthly via conference call. The clinical specialist represents the satellites, with the ability to communicate practice questions, quality concerns and policy interpretations that transpire from the committee’s monthly items to Boston colleagues via committee representation and collegial discussion. The clinical specialist reports back to the committee results or possible policy and practice changes.
Results: The committee initially met in April 2017. The work that the committee has accomplished has been tremendous in a short amount of time, including Hypersensitivity note sheets, patient teach checklists, primary nursing assignments, and shared care guidelines. The meeting agenda and minutes are compiled and disseminated at each satellite location via monthly staff meetings.
Conclusions: The practice changes that the committee has influenced include, waste disposal standardization, review of initial nursing assessment, and primary nursing assignments. The staff report feeling more connected to Boston and state that the committee is an important vehicle to enhance communication between the satellite locations and the Boston campus.
Analysis of Next Generation Sequencing results for Pathogenic gene mutations*
S. Mahmood, J. He, F. De Abreu, S. Deharvengt, J. Peterson, H. Steinmetz, W. Wells, G. Tsongalis
Dartmouth Hitchcock Medical Center and Norris Cotton Cancer Center
Background: Next generation sequencing (NGS) assays were developed to screen for somatic variants in multiple cancer types on a much larger scale than previously done using other methods such as Fluorescence in situ hybridization (FISH) and real time PCR. These somatic variant analyses have become critical in treatment and management of these cancers. In this study we present somatic variant data identified in lung, colorectal, breast, melanoma and glioma.
Methods: Data was obtained from over 2500 FFPE samples screened for somatic mutations using the Ampliseq Cancer Hotspot Panel v2. Ten nanograms of genomic DNA was used to prepare barcoded libraries for sequencing using Ion PGM System. The variants detected were classified into two categories: (1) Actionable (genes for which FDA- approved treatment exists), and (2) Non-actionable (no FDA approved treatment).
Results: A total of 3550 variants were identified in the 2500 cases. The following actionable somatic variants were found from a total number of variants: 10/42 (24%) breast, 389/1543 (25%) colorectal, 83/288 (29%) glioma, 518/1378 (38%) lung, and 140/299 (47%) melanoma. TP53 was the most commonly identified mutation in breast, colon, glioma and lung tumors followed by PIK3CA in breast, KRAS in colorectal, IDH1 in glioma, KRAS in lung and NRAS in melanoma.
Conclusions: NGS has become a standard part of the pathologic workup for human cancers that can identify variants in multiple genes simultaneously. These genomic profiles can be used for optimization of therapeutic selection.
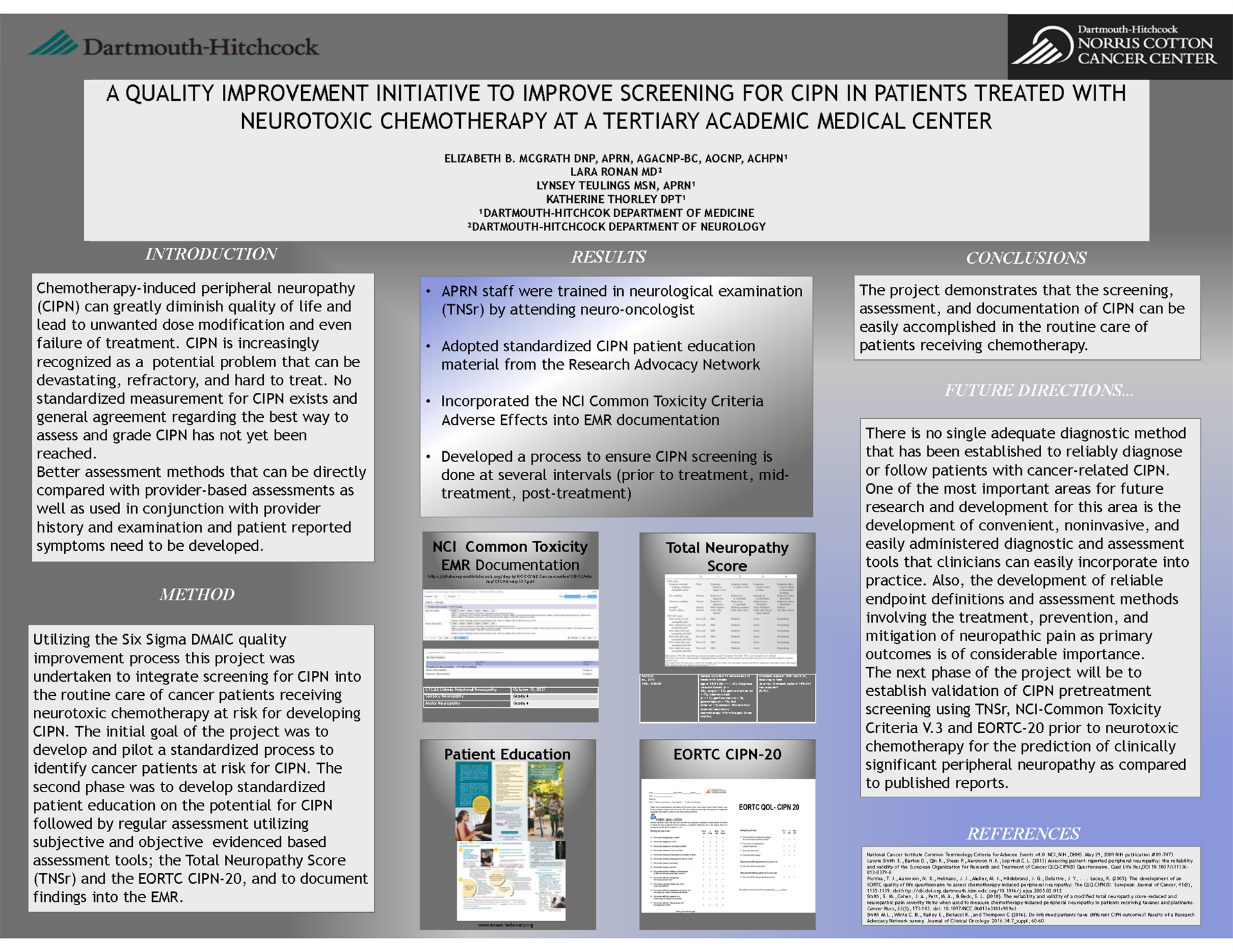
Establish Validation of CIPN Pretreatment Screening using TNSr, NCI-Common Toxicity Criteria V.3 and EORTC-20 prior to neurotoxic chemotherapy
E. McGrath¹, L. Ronan², L. Teulings¹
¹Dartmouth-Hitchcok Dept of Medicine; Dartmouth-Hitchcock Dept of Neurology
Background: Chemotherapy-induced peripheral neuropathy (CIPN) can greatly diminish quality of life and lead to unwanted dose modification and even failure of treatment. CIPN is increasingly recognized as a problem that can be devastating, refractory, and hard to treat. No standardized measurement for CIPN exists and general agreement regarding the best way to assess and grade CIPN has not yet been reached.
Methods: A quality improvement project was undertaken to integrate screening for CIPN into the routine care of patients receiving neurotoxic chemotherapy at risk for developing CIPN. The goals of the project was to develop and pilot a standardized process to identify cancer patients at risk for CIPN, standardized patient education on the potential for CIPN followed by regular assessment utilizing subjective and objective evidenced- based assessment tools, the Total Neuropathy Score (TNSr) and the EORTC CIPN-20. The project demonstrated screening for CIPN can be easily accomplished by APRN’s in the routine care of patients receiving chemotherapy.
Results: As a result of this work the neurologist trained the APRN staff in neurological examination and we adopted CIPN patient education material into patient visits, incorporated the NCI Common Toxicity Criteria into the EMR for documentation, and developed a process to ensure CIPN screening is done at the several intervals.
Conclusions: The next phase of the project will be to establish validation of CIPN pretreatment screening using TNSr, NCI-Common Toxicity Criteria V.3 and EORTC-20 prior to neurotoxic chemotherapy for the prediction of clinically significant peripheral neuropathy as compared to published reports.
 Radioactive seed versus wire guided localization in breast lumpectomy: analysis of pathologic factors and adequacy of excision
Radioactive seed versus wire guided localization in breast lumpectomy: analysis of pathologic factors and adequacy of excision
A. Meader1, W. Jones2, P. Teller1, M. Jones1
1Maine Medical Center; 2University of Colorado Anschutz Medical School
Background: The introduction of I125 radioactive seed (RSL) localization for surgical excision of breast lesions demonstrates an improvement in patient satisfaction and eases procedural scheduling compared to same-day wire-guided localization (WGL). A paucity of data exists comparing the pathologic features of lumpectomy specimens using these techniques with regards to excision volume, margin status and re-excision rates. We report the experience of the ambulatory surgery center at Maine Medical Center in transitioning from WGL to RSL.
Methods: A retrospective chart review was conducted of the last 80 patients undergoing WGL and the first 80 RSL patients. Patients with benign pathologic diagnoses were excluded, leaving 75 RSL and 66 WGL patients. Tumor size, histologic subtype, lumpectomy size, final margin status, and need for additional surgery were reviewed.
Results: There was comparable tumor size at 1.3 cm WGL versus 1.1cm RSL (p=.496) and distribution of histology types between groups (IDC p=.534, ILC p=1.0, DCIS p=.651). Lumpectomy volume was 109cm WGL and 98cm RSL (p=.547). No difference was found in WGL versus RSL final margin status rates: positive (5.2% vs 9.1%, p=.544), close (<1mm) (26% vs 29%, p=1.00) and negative (64% vs 62%, p=1.00). Additional surgery with re-excision was performed 0.8% of WGL and 1.0% RSL cases (p=.966). Completion mastectomies were performed in 12% WGL and 17% RSL cases (p=.553).
Conclusions: No significant differences were found between the two cohorts with respect to all variables analyzed. Results demonstrate RSL is equivalent to WGL in performance while offering increased patient comfort and case scheduling flexibility.
 Influence of patient navigators on care coordination within an institutional Lynch syndrome screening program
Influence of patient navigators on care coordination within an institutional Lynch syndrome screening program
S. Miesfeldt1, W. G. Feero2, F. Lucas3, K. Rasmussen4
1Cancer Risk and Prevention Program, Maine Medical Center; 2Maine-Dartmouth Family Medicine Residency, MaineGeneral Health; 3 Center for Outcomes Research and Evaluation, Maine Medical Center; 4Clinical Molecular Genetics, Maine Medical Center
Background: Lynch syndrome (LS) identification improves health outcomes in individuals/families. Universal tumor screening (UTS) through immunohistochemical (IHC) and/or microsatellite instability (MSI) testing facilitates LS identification among colorectal cancer (CRC) and uterine cancer (UC) patients. Institutional interdisciplinary case management is necessary for effective LS screening outcomes. Study of institutional care coordination needs is limited, including the impact of patient navigation on follow-through to genetic services among screen-positive patients.
Methods: Institutional electronic health record review of LS screen-positive CRC and UC cases for twelve months assessed the relationship between patient navigation and follow-through to cancer genetic counseling/testing.
Results: Among 451 patients with newly diagnosed CRC (n=175) and UC (n=276), 96 (21.3%) had abnormal UTS results, including 2 with incomplete results. Sixty-six (68.8%) of these were the result of MLH1 promoter hypermethylation. Of the remaining 30 screen-positive cases, 16 received navigation services; 14 did not. Among navigated patients, 14/16 (87.5%) underwent cancer genetic counseling and of these, 12 elected genetic testing; one additional patient was tested via oncologist. Among those tested, 53.8% had pathogenic/likely pathogenic variants. Among non-navigated patients, 2/14 had incomplete UTS results. Five of the remaining 12 cases (41.7%) received genetic counseling services; four elected genetic testing; 1/4 (25%) tested positive.
Conclusions: Involvement of patient navigators appears to be associated with follow-through to cancer genetic counseling/testing services among LS screen-positive cases. Future studies are necessary to determine whether this association is causal.
 Drug-Anticoagulant Interactions in Cancer Patients at High Risk for Venous Thromboembolism Initiating Outpatient Chemotherapy
Drug-Anticoagulant Interactions in Cancer Patients at High Risk for Venous Thromboembolism Initiating Outpatient Chemotherapy
H. Ng1, B. Rogala2, J. Schwartz³, T. Ahikaga⁴, S. Ades¹, C. Holmes¹
¹University of Vermont Medical Center; ²College of Pharmacy, University of Rhode Island ; ³Albany College of Pharmacy and Health Sciences; ⁴University of Vermont Medical Biostatistics
Background: Drug options for VTE prophylaxis are varied and limited data is available on the potential drug interactions commonly encountered in cancer outpatients. Information regarding drug-anticoagulant interactions and their relationship to VTE and bleeding is needed to improve care.
Methods: Based on a prospective VTE risk assessment program at UVM, 108 high-risk cancer patients were identified between October 2015 and September 2016 and underwent chart review. Drug interactions were ascertained by pharmacists using a checker tool based on current medications and anticoagulant prescribed, and then graded on a scale of C, D, and X – with X meaning the combination is contraindicated. A cross sectional analysis was performed that included VTE and bleeding endpoints within one year.
Results: An average of 0.92 apixaban-drug interactions (range 0-2); 0.66 (range 0-2) rivaroxaban-drug interactions; 2.7 (range 0-6) warfarin-drug interactions; and 0.97 (range 0-5) LMWH-drug interactions were found per patient. For apixaban, 2% of interactions were grade X, 0% grade D, 67% grade C; for rivaroxaban, 2% grade X, 1% grade D, 62% grade C; for warfarin, 0% grade X, 23% grade D, 95% grade C; and for LMWH, 0% grade X, 49% grade D, 30% grade C. With 11 bleeds and 7 VTEs, no increased risk of bleeding or thrombosis was found with any specific anticoagulant.
Conclusions: The anticoagulant class with the least number of interactions in cancer outpatients was DOAC therapy. There was no difference in VTE or bleeding events between anticoagulants.
 Effect of Tumor Volume Doubling Time (VDT) on Prognosis for Stage I Non-Small Cell Lung Cancer: An Update*
Effect of Tumor Volume Doubling Time (VDT) on Prognosis for Stage I Non-Small Cell Lung Cancer: An Update*
H.No1, D. Seward2, T. Ashikaga3, M. Kinsey4, N.Sidiropoulos2, H. Gagne5, C. Nelson5, J. Kikut6, G. Gentchos7, G. Garrison4, E. Folefac8, B. Leavitt9, K. Dragnev10, S. Lin11, C. Anker5
¹The University of Vermont Larner MD College of Medicine; ²Department of Pathology and Laboratory Medicine, University of Vermont Medical Center; ³College of Engineering and Mathematical Sciences, University of Vermont; ⁴Division of Pulmonary and Critical Care Medicine, University of Vermont Medical Center; ⁵Division of Radiation Oncology, University of Vermont Cancer Center;⁶Nuclear Medicine and Diagnostic Radiology, University of Vermont Medical Center; ⁷Department of Radiology, University of Vermont Medical Center; ⁸Department of Hematology and Oncology, University of Vermont Cancer Center; ⁹Division of Cardiothoracic Surgery, University of Vermont Medical Center; 10Norris Cotton Cancer Center, Dartmouth-Hitchcock Medical Center; 11Department of Radiation Oncology, The University of Texas MD Anderson Cancer Center
Background: Computed tomography (CT)-based screening for early detection of non-small cell lung cancers (NSCLC) may improve overall survival (OS). However, some tumors exhibit indolent growth necessitating additional prognostic indicators. Data supporting the prognostic value of tumor volume doubling time (VDT) was presented at the 2016 NNECOS meeting; 4 additional years of data, gathered to better assess VDT impact, are presented here.
Methods: A retrospective review identified 433 patients from UVM treated for Stage I NSCLC, diagnosed between 2010-2015, of whom 67 met the following criteria for this study: ≥1 year follow-up and ≥3 month interval between ≥2 CT scans prior to treatment. CT-based VDT calculation used a modified Schwartz equation for exponential growth. Other prognostic factors evaluated included age, stage (IA vs. IB), histology and treatment. OS and disease-free survival (DFS) were evaluated by the Kaplan-Meier Method and Cox proportional hazard models.
Results: Median follow-up for living patients was 46.2 months, and median age was 71. Stage IA disease (88%) and adenocarcinoma (79%) predominated. Forty-one patients underwent surgery, 21 received radiation, and 5 received radiofrequency ablation. Forty-nine percent exhibited VDT ≥400 days. Four-year DFS was superior at 100% for VDT ≥400 days vs. 50% if VDT <400 days (p<.0001). No other factor correlated with DFS or OS. All 15 patients with recurrences had VDTs <400 days, with a local component in 10, regional in 4, and distant in 6.
Conclusions: Results support VDT correlates with prognosis in Stage I NSCLC, as all patients who recurred demonstrated reduced VDT (<400 days).
 Enhancing Bone Marrow Transplant Care through the Patient Experience
Enhancing Bone Marrow Transplant Care through the Patient Experience
A.Prokopik1, L. Wesinger2, C. Morton2, J. Holl2, J. Gentes2, S. Rossi2, S. Smith2, A. Riley2
S. Aldrich2, M. Bennett2, J. Coffey², J. Hill, Jr.2
¹Dartmouth Hitchcock / University of New Hampshire; 2Department of Hematology/Oncology, Dartmouth-Hitchcock Medical Center; 3Center for Nursing Excellence, Primary Care Pediatrics, Dartmouth-Hitchcock Medical Center
Background: Education of health care providers has traditionally utilized case studies to present a clinical platform for discussion of specific medical issues and the method of addressing them. This training process has generally been objective and de-personalized, without incorporating individual patient perspectives on illness or related therapy. As healthcare evolves towards a more holistic-based system, there is a growing awareness that our educational methods for healthcare providers must be broadened to keep pace with this innovation. Our team therefore sought to move beyond the traditional case study method of bone marrow transplant (BMT) nursing education in favor of a more patient-centered approach.
Methods: This teaching method involves embedding the patient’s personal experience and constructive feedback into the existing educational format. This is being undertaken through voluntary interviews of BMT recipients and their caregivers, spanning from the pre-transplant discussion and preparation for inpatient hospitalization through the period of post-transplant recovery and extended follow up. A total of eight patient-caregiver pairs are participating, each pair representing a unique facet of transplant.
Results: Testing options are currently being considered to optimally assess the educational benefit of this intervention. It is hoped that this model will provide a uniquely insightful learning tool for providers that goes well beyond the traditional diagnosis-based method.
Conclusions: Development of a new, patient-centered teaching modality has the potential to revolutionize provider education. The prospect of extending this approach to other facets of clinical training (non-BMT nursing, medical housestaff and students, and even ancillary providers), is exhilarating.
 Lynch associated adrenocortical tumor with a rare MSH6 pathogenic variant
Lynch associated adrenocortical tumor with a rare MSH6 pathogenic variant
B. Pulluri, W. McKinnon, A. Kalof, M. Greenblatt, S. Ades
University of Vermont Medical Center
Background: Adrenocortical carcinoma (ACC) is a rare endocrine cancer with an incidence of 1-2 cases/million individuals/year. 3-5% of adult ACC are associated with genetic syndromes. Given the rarity of ACC, its association with Lynch syndrome (LS) has not been well described. A 3.2% prevalence of Lynch-associated ACC was reported in a recent prospective series of 114 ACCs.
Methods: We report a case of LS-associated ACC with a rare novel MSH6 variant.
Results: A 2 cm right adrenal nodule and a small left adrenal nodule, both deemed benign, were found incidentally in a 37-year-old woman. In five years, the left adrenal nodule grew to 3x3x4 cm. Laparoscopic left adrenalectomy showed a 4 cm ACC, stage I, proliferative index 60-70%, 21 mitoses/10 high power fields. Adjuvant mitotane therapy was commenced, but was discontinued due to liver dysfunction and cirrhosis.
Family history: Proband’s mother had endometrial cancer and maternal aunt had bladder cancer. Genetic testing revealed an MSH6 pathogenic frame shift variant, c.908dupT (p.M303Ifs*9). Immunohistochemistry testing showed loss of MSH6 protein with intact MSH2, MLH1, and PMS2. The MSH6 variant was identified in two siblings. Proband’s sister had an adrenal nodule that was resected and was benign.
Conclusions: We report the rare occurrence of ACC in MSH6-associated LS. Given the low incidence of ACC, determining the association with LS has been controversial. In the absence of well-defined criteria for Lynch screening in ACC, personalized screening of carriers may provide optimal care when clinical association is suspicious.
 The Nurses’ Self-Efficacy Project
The Nurses’ Self-Efficacy Project
J. Pushee1, J. Coffey², E. McGrath²
¹Colby-Sawyer College; ²Dartmouth-Hitchcock Medical Center
Background: For the past 7 years, Dartmouth College INBRE (Idea Network of Biomedical Research Excellence) and Dartmouth-Hitchcock have collaborated to offer 4-5 junior and senior nursing students a summer research internship with the goal to expand the individual intern’s capacity for research. The program is unique as it is the only INBRE program nationally that offers this internship to nursing students. The students complete various evaluations regarding the program experience, however prior to 2016 there was no evaluation of the program’s potential to build research self-efficacy. The specific aim of this research pilot study is to assess if the summer nursing research internship has a positive impact on individual nursing intern’s research self-efficacy.
Methods: The Nursing Research Self-Efficacy Scale (NURSES), using a 5-point Likert scale, asks about the level of confidence to complete various research activities. The final part of the survey (10 questions) was omitted as it is not applicable to the student experience. The pilot study had IRB approval and the questionnaires were administered at the beginning and the end of the 10 week summer research internship using the RedCap survey platform.
Results: Results from the participants are being analyzed.
Conclusions: The findings from the pilot study on nurse research intern self-efficacy will be used to evaluate the current summer learning plan and guide future curriculum planning for the nursing INBRE program.
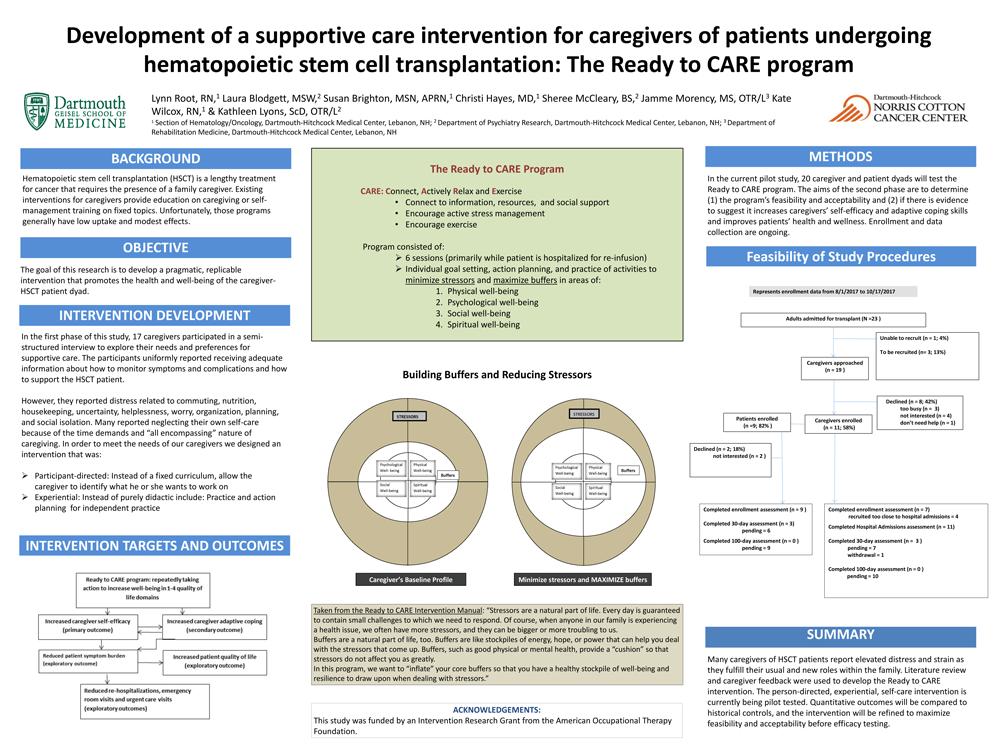
Development of a supportive care intervention for caregivers of patients undergoing hematopoietic stem cell transplantation: The Ready to CARE program
L. Root¹, L. Blodgett², S. Brighton¹, C. Hayes¹, J. Morency³, K. Wilcox1, L. Lyons²
¹Department of Hematology/Oncology, Dartmouth-Hitchcock Medical Center; ² Department of Psychiatry Research, Dartmouth-Hitchcock Medical Center; ³Department of Rehabilitation Medicine, Dartmouth-Hitchcock Medical Center
Background: Hematopoietic stem cell transplantation (HSCT) is a lengthy treatment for cancer that requires the presence of a family caregiver. The goal of this research is to develop a pragmatic, replicable intervention that supports caregivers and promotes the health and well-being of the caregiver-HSCT patient dyad.
Methods: In the first phase of this study, 17 caregivers participated in a semi-structured interview to explore their needs and preferences for supportive care. In the second phase of the study, 20 caregiver and patient dyads will test a new intervention called the Ready to CARE program. The aims of the second phase are to determine (1) the program’s feasibility and acceptability and (2) if there is evidence to suggest it increases caregivers’ confidence and adaptive coping skills and improves patients’ health and wellness.
Results: The Phase 1 participants uniformly reported receiving adequate information about how to monitor symptoms and complications and how to support the HSCT patient. However, they reported distress related to commuting, nutrition, housekeeping, uncertainty, helplessness, worry, organization, planning, and social isolation. Many reported neglecting their own self-care because of the time demands and “all encompassing” nature of caregiving.
Conclusions: Many caregivers of HSCT patients report elevated distress and strain as they fulfill their usual and new roles within the family. Results of the Phase 1 interviews were used to develop the Ready to Connect, Actively Relax, and Exercise (Ready to CARE) intervention. The person-directed, experiential, self-care intervention is currently being pilot tested.
 Potential herb-chemotherapy or radiation interactions in patients with cancer: A prospective study of the pharmacist and student-pharmacist run herbal assessment service at the University of Vermont (UVM) Cancer Center
Potential herb-chemotherapy or radiation interactions in patients with cancer: A prospective study of the pharmacist and student-pharmacist run herbal assessment service at the University of Vermont (UVM) Cancer Center
J. Schwartz, A. Tran
Albany College of Pharmacy and Health Sciences-VT campus
Background: While the use of herbals is increasing, they are still not included in computer interaction checker tools. This study aimed to identify the incidence of herbal-chemotherapy or radiation interactions and measure patient satisfaction with a service that researches and communicates these interactions to patients/providers.
Methods: Following IRB approval, consenting new patients receiving first-dose IV chemotherapy (+/- radiation) for one year were surveyed for herbal usage. The pharmacy team used online herbal sources to identify interactions involving overlapping toxicities, antagonism of therapy mechanism, or metabolic (cyp450) interactions with therapy, communicated them to the patient/provider, and then supplied a validated satisfaction survey. Regression analysis was performed to identify variables associated with risk for interactions.
Results: In 1 year, 98.8% (320) of 324 patients consented, and 38% reported using herbals. Of those reporting herbal use, 56% were on 5+ herbals, and 305 total interactions were identified. Of the 73% of patients who had at least one interaction, 98% of those agreed to stop all interacting herbals. Herbal assessment required a mean of 47 min. of research (range 0.5-3 hours) using multiple sources. All patients who returned surveys (n=52) indicated five (highly satisfied) for every parameter, whether the communication was by the pharmacist or student. Risk of interactions was associated with use of 5+ herbals (OR 2.53, CI 1.08-5.91. P=0.03.)
Conclusions: Herbal-chemotherapy or radiation drug interactions are frequent. Student-pharmacists can be trained to fulfill a needed service with high patient satisfaction that would be very time-consuming for providers, since current computer checkers do not flag these interactions.
HWright_Foundation Study NNECOS - FINAL.pdf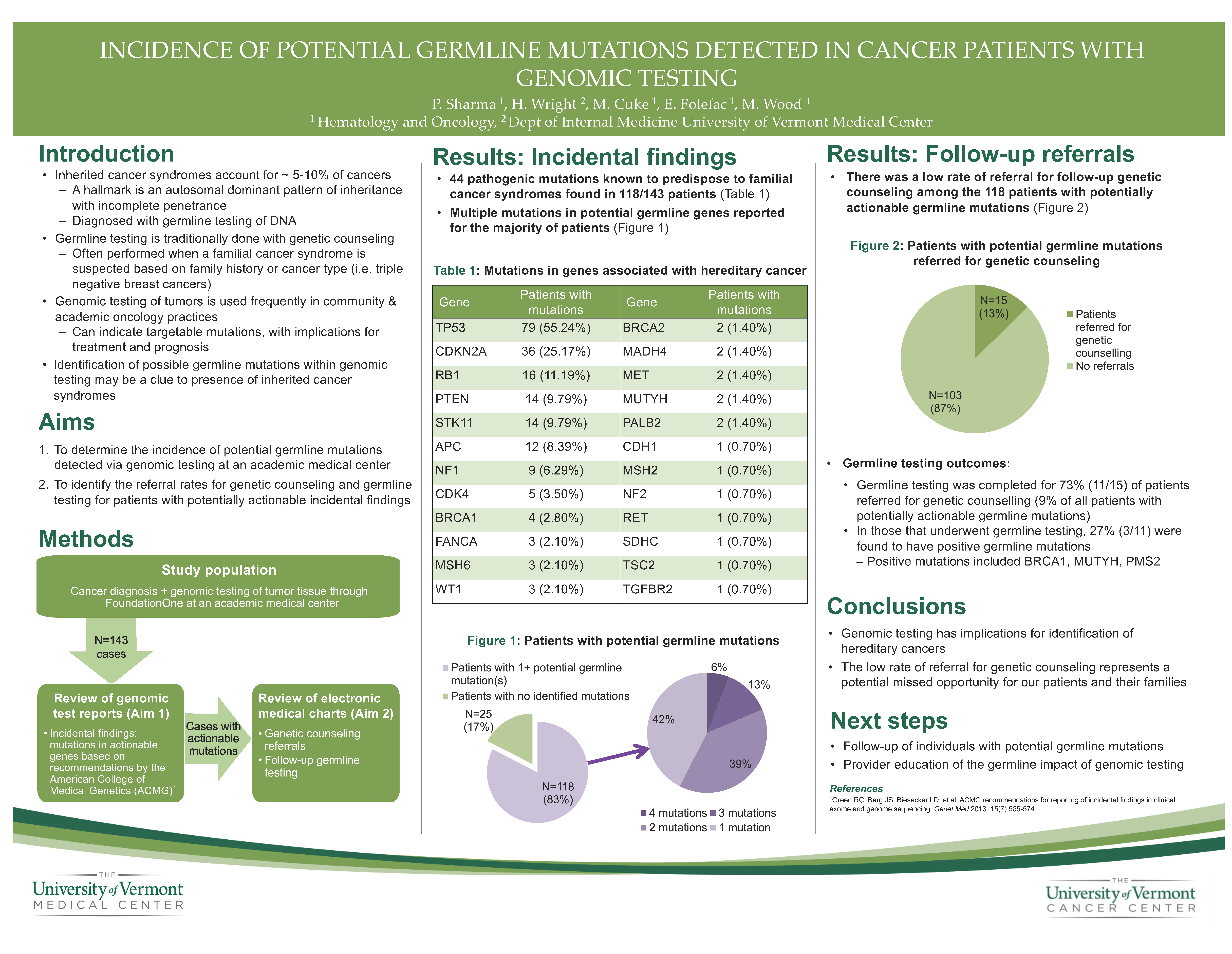
Incidence of Potential Germline Mutations in Cancer Patients with Genomic Testing
P. Sharma, H. Wright, M. Sands, E. Folefac, M. Wood
University of Vermont Cancer Center
Background: Genomic sequencing has implications for treatment and prognosis, and is being used frequently in community and academic oncology practices. However, genomic testing can be a clue to the presence of an inherited cancer syndrome. We sought to determine the incidence of germline findings within individuals undergoing genomic testing at our center and evaluate the referral rate of these individuals for genetic counseling.
Methods: A retrospective chart review of patients who have undergone genomic testing at UVM Cancer Center was performed. Gene mutations recognized by ACMG as being actionable (including PALB2) were identified from Foundation One reports. Rates of germline testing and genetic counselling referral were collected from patients’ electronic medical records.
Results: 143 reports were identified and reviewed. Pathogenic mutations in 44 genes known to predispose to familial cancer syndromes were found in 118 patients. The most common mutations were found in TP53 (79), CDKN2A (36), PTEN (14), RB1 (16) the majority of which (but not all) are likely somatic. Mutations were also found in BRCA1 (4), BRCA2 (2), PALB2 (2), MSH2 (1), MSH6 (3) and are likely germline. 15/118 (12.7%) have been referred for genetic counseling and testing was performed in 11 (9.3%). 3/11 (27%) patients had positive germline mutations.
Conclusions: Our study highlights the implications of genomic testing in identification of hereditary cancer. The low rate of referral for genetic counseling represents a potential missed opportunity. Next steps will focus on follow-up of individuals with potential germline mutations and provider education of the germline impact of genomic testing.
Targeting CLL and MCL cells with DNA repair and B cell receptor inhibitors
L. Shopland¹, A. Curtis¹, A. Moineau1,2, D. Pham 1,2, S. Rajan¹, R. Zhang¹, E. Brooks¹, T. Hoffert¹, J. Rueter¹
¹Eastern Maine Medical Center Cancer Care; 2University of Maine, Orono
Background: Patient-specific responses and the development of ibrutinib resistance remain significant challenges to the treatment of mantle cell lymphoma (MCL) and chronic lymphocytic leukemia (CLL). The poly ADP ribose polymerase (PARP) inhibitor, olaparib, targets cells with high levels of DNA damage, which have the mutational potential to become drug resistant.
Methods: To improve treatment efficacy and delay ibrutinib resistance, we tested ibrutinib treatment with olaparib on CLL and MCL cells in vitro. Primary CLL cells from patients were obtained via collaboration with the Harold Alfond Center for Cancer Care. These and MCL cell lines were analyzed by indirect immunofluorescence, cell counting, and flow cytometry.
Results: CLL cells were found to have significant patient-to-patient differences in their levels of DNA damage. These differences correlate with increased copies of the gene, AICDA. Limitations in primary CLL cell culture have prevented testing of ibrutinib plus olaparib thus far. However, tests of these drugs on MCL cell lines revealed either additive or synergistic inhibition of culture growth. These effects correlate with the absence and presence of the DNA repair protein, ATM, respectively.
Conclusions: Our data provide a strong case for investigation of olaparib-ibrutinib combination therapy in MCL and CLL animal models. The additive and synergistic inhibitions of tumor cell growth support a therapeutic strategy using lower doses of each drug in combination to reduce side effects. Our data also suggest that the expression of AID and ATM might be useful biomarkers for this combination therapy in CLL and MCL, respectively.
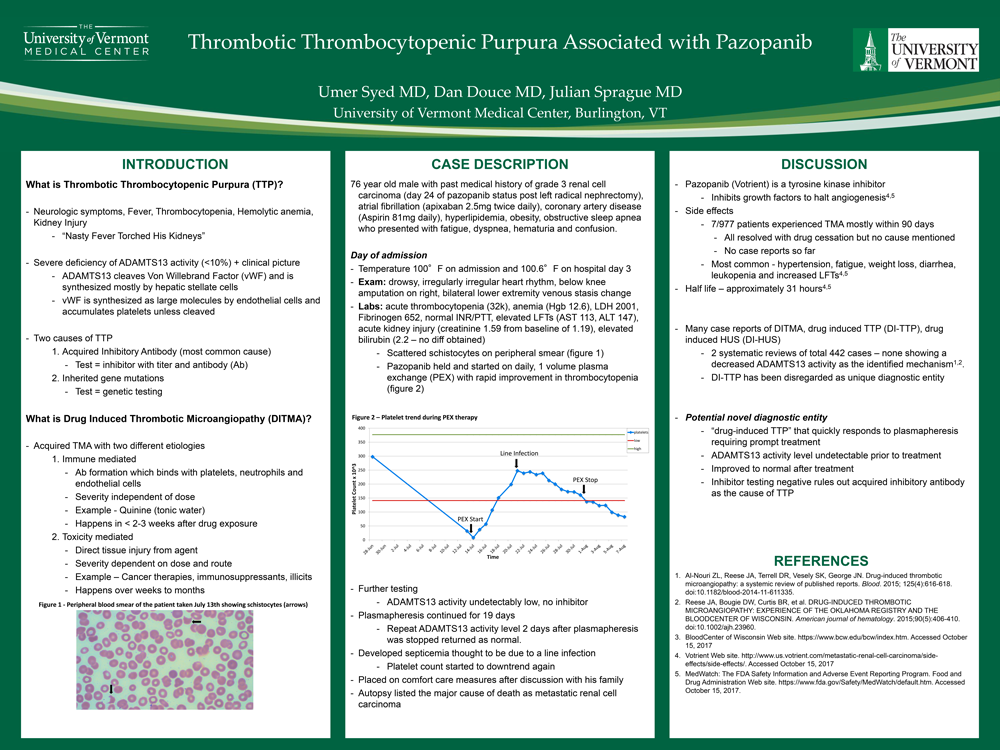
Thrombotic Thrombocytopenic Purpura Associated with Pazopanib
U. Syed, D. Douce, J. Sprague, University of Vermont Medical Center
Background: A 76 yo male with metastatic clear cell renal carcinoma on day 24 of Pazopanib was admitted with complaints of nausea, emesis, confusion and hematuria. Lab testing showed an acutely elevated serum creatinine, LDH, total bilirubin, and a platelet count of 32 k/m3. Scattered schistocytes were seen on peripheral smear and he was diagnosed with thrombotic microangiopathy (TMA). He was subsequently started on daily, 1 volume plasma exchange with rapid improvement in thrombocytopenia.
His platelet count normalized and ADAMTS13 activity returned as undetectably low with no inhibitor detected. Plasmapheresis was continued for 19 days, as he had become febrile and confused on days when plasmapheresis was held. Repeat ADAMTS13 activity level 2 days after plasmapheresis was stopped returned as normal. His platelet count remained stable after stopping plasmapheresis, but started to downtrend within 4 days. He developed septicemia thought to be due to a line infection, and developed arrhythmias. He was placed on comfort care measures after discussion with his family. An autopsy listed the major cause of death as metastatic renal cell carcinoma.
Conclusions: According to 2 separate meta analyses, none of the proven drug induced TMA cases had a decreased ADAMTS13 activity as the identified mechanism. While Pazopanib is also associated with TMA, this unique case suggests a novel potential mechanism for TMA associated with Pazopanib and brings forth “drug-induced TTP” as a possible new diagnostic entity that quickly responds to plasmapheresis requiring prompt recognition and treatment.
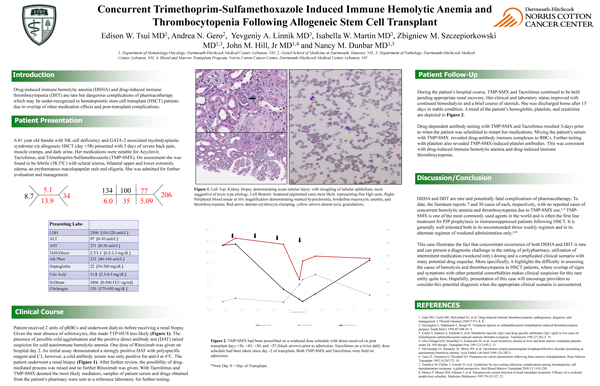
Concurrent Trimethoprim-Sulfamethoxazole Induced Immune Hemolytic Anemia and Thrombocytopenia Following Allogeneic Stem Cell Transplant
E. Tsui¹, A. Gero², Y. Linnik³, I. Martin³, Z. Szczepiorkowski1,3, J. Hill, Jr1,4, N. Dunbar 1,3
¹Department of Medicine, Dartmouth-Hitchcock Medical Center; ²Geisel School of Medicine at Dartmouth; ³Department of Pathology and Laboratory Medicine, Dartmouth-Hitchcock Medical Center; ⁴Blood and Marrow Transplant Program, Norris Cotton Cancer Center, Dartmouth-Hitchcock Medical Center
Background: Drug-induced immune hemolytic anemia (DIIHA) and drug-induced immune thrombocytopenia (DIIT) are rare but dangerous complications of pharmacotherapy which may be under-recognized in hematopoietic stem cell transplant (HSCT) patients due to overlap of other medication effects and post-transplant complications.
Methods: A 61 year old woman with GATA-2 mutation and associated NK-cell deficiency and myelodysplastic syndrome underwent a matched-related HSCT. Her post-transplant course was uncomplicated until day +58, when she presented with severe back pain, muscle cramps and increasingly dark urine. She was found to be anemic, thrombocytopenic, and in acute renal failure. Serologic peripheral blood testing was performed using standard methods, with drug studies sent to an outside immunohematology reference laboratory.
Results: On admission, the direct antiglobulin test was positive for complement (C3) only. After careful review of her medications, the possibility of DIIHA was raised. She had initiated trimethoprim-sulfamethoxazole (TMP-SMX) for Pneumocystis jiroveci pneumonia prophylaxis 24 days prior on a weekend dose schedule. The patient’s serum showed hemolysis of donor red cells in the presence of TMP-SMX and also TMP-SMX-induced antiplatelet antibodies. She was treated with transfusions, hemodialysis, and immunosuppressive agents. Her condition improved and she was discharged after 8 days in stable condition.
Conclusions: This is the first reported case of concurrent DIIHA and DIIT due to TMP-
SMX-induced antibodies in a HSCT patient. This illustrates the fact that DIIHA and DIIT can present a diagnostic challenge in the setting of polypharmacy, utilization of intermittent medication dosing and a complicated clinical scenario with many potential non-drug sequelae.
 Evaluation of Kindred Connections cancer survivor peer support program
Evaluation of Kindred Connections cancer survivor peer support program
A. Verbyla¹, J. Chu², D. Cranmer³, S. Mallory¹, A. Johnson¹
¹Vermont Department of Health; ²John Snow, Inc.; ³Vermont Cancer Survivor Network
Background: The population of U.S. cancer survivors is projected to increase to 20.3 million by 2026 (ACS). About one out of every seven cancer survivors suffers from low emotional support and poor mental health. Peer support is vital to address the growing needs of this unique population. Kindred Connections (KC) is a peer-to-peer support system in the state of Vermont that pairs cancer survivors (volunteers) with those who have a more recent diagnosis of cancer (participants).
Methods: A qualitative study was conducted in early 2017. A focus group of KC volunteers was recruited during the 2016 KC celebration. Eight out of 33 potential volunteers were interviewed. Recruitment of KC participants was done through the KC coordinator. Of 12 potential participants, eight agreed to an interview. Interviews were transcribed, and transcriptions were reviewed for common themes.
Results: Emergent themes from KC volunteers include a benefit of giving back to the cancer community and the ease of creating connections outside of social boundaries. KC participants valued creating connections based on a shared experience and a chance for one-on-one attention from someone outside of their support circle. KC participants also felt that this program served as a vital source of local resources for cancer patients.
Conclusions: Both volunteers and participants expressed that being part of Kindred Connections greatly improved their quality of life. Both groups valued the flexibility and organic nature of the connections. It was recommended that the volunteer base receive further training and be more diverse.
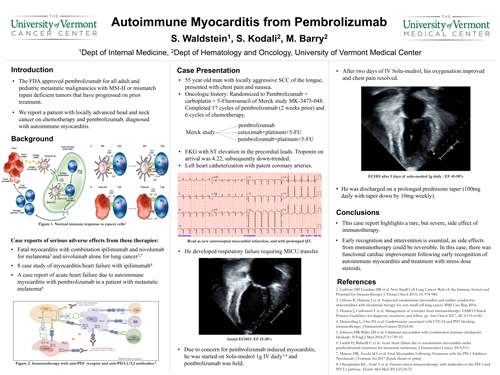
Acute Heart Failure due to Autoimmune Myocarditis from Pembrolizumab
S. Waldstein, S. Kodali, M. Barry
University of Vermont Medical Center
Background: Immunotherapy was successfully introduced into oncological practice and recently F.D.A approved pembrolizumab for all adult and pediatric metastatic malignancies with MSI-H or mismatch repair deficient tumors that have progressed on prior lines of treatment. With immunotherapy increasingly replacing cytotoxic chemotherapy, it is important to monitor for adverse effects. We report a patient with locally advanced head and neck cancer who was enrolled in MK-3475 trial with chemotherapy plus pembrolizumab and presented with chest pain, diagnosed with autoimmune myocarditis.
Methods: 55-year-old smoker was diagnosed with stage IVA squamous cell carcinoma of base of the tongue. Patient received concurrent chemo-radiation with good response. Unfortunately, he developed recurrent squamous cell carcinoma. Patient was enrolled in Merck study MK-3475 and was randomized to chemotherapy plus immunotherapy arm. He presented to our hospital with chest pain and shortness of breath after 17 cycles.
Results: An ECG revealed acute ST elevations in the precordial leads. Patient was started on heparin drip and was emergently transferred to the cath-lab where he was found to have non-occlusive disease. An Echocardiogram revealed dilated left ventricle with severely depressed ejection fraction (EF) at 15%. His acute cardiomyopathy is secondary to autoimmune myocarditis from pembrolizumab. Patient received high-dose steroids with solumedrol 1 gm IV daily which was transitioned to oral prednisone. He was discharged and repeat echo showed improved EF at 60%.
Conclusions: This case report highlights a rare but severe side effect of immunotherapy. Documentation of these cases is helpful for early recognition and to guide successful early interventions.
 Clinical Utility of PET/CT in Non-Small Cell Lung Cancer
Clinical Utility of PET/CT in Non-Small Cell Lung Cancer
G. Wasp, C. Del Prete, J. Farrell, K. Dragnev, G. Russo, G. Atkins, G. Brooks
Dartmouth-Hitchcock Medical Center
Background: PET/CT is a routine and costly part of the pretreatment evaluation of non-small cell lung cancer (NSCLC). We hypothesized that there is a subset of patients for whom PET/CT does not significantly alter clinical staging.
Methods: We conducted a retrospective chart review of all patients with a new diagnosis of NSCLC from January 1st to December 31st, 2015. We excluded patients with recurrent NSCLC, multiple cancers, or incomplete records. Data collected included demographics, stage and histology, PET/CT results, conventional imaging results prior to PET/CT, presence of bone metastasis, malignant effusions, and hospital setting. Use of PET/CT was assessed in two patient groups, based on evaluation completed prior to PET/CT: 1) peripheral stage Ia, 2) suspected or confirmed stage IV (pathologically confirmed malignant effusions, multiple bony metastases, or ≥2 suspected metastatic sites).
Results: A total of 216 patients were included for analysis: 193 had a PET/CT performed (89%). 54 patients had suspected stage IV disease prior to PET/CT ; of these 38 (70%) went on to have a PET/CT, and only 2 patients (3.7%) had disease stage changed based on PET/CT results. 40 patients with peripheral stage Ia disease were evaluated, of whom 39 had a PET/CT. In 2 cases (5%) disease stage was changed.
Conclusions: At our center, PET/CT changed staging in ≤5% of patients with pre-PET stage Ia or stage IV NSCLC. These populations comprise over 40% of NSCLC diagnoses, and the utility and value of PET/CT in these patients is uncertain.
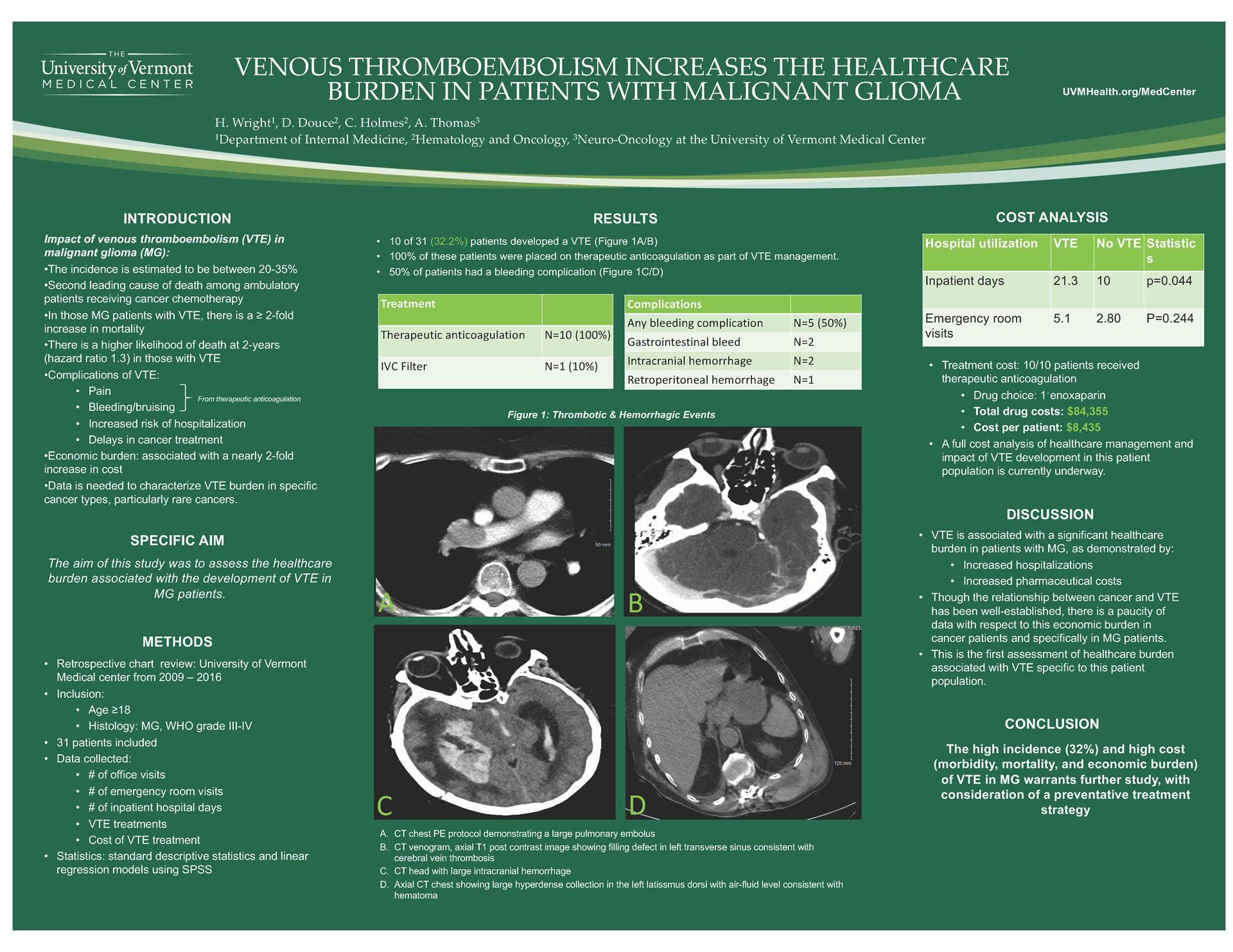
Venous Thromboembolism (VTE) Increases the Healthcare Burden in Patients with Malignant Glioma (MG)
H. Wright, D. Douce, C. Holmes, A. Thomas
University of Vermont Medical Center
Background: The cumulative incidence of symptomatic VTE among patients with MG is high, with estimates ranging from 20-35%. The economic burden of VTE in cancer patients is substantial and is associated with a nearly 2 fold increase in cost.
Methods: A retrospective chart review of patients with MG at UVMMC was conducted from 2009-2016. Patients 18 years and older with a histologic diagnosis of malignant glioma, WHO grade 3-4 were assessed. A total of 31 patients were identified and the number of office and emergency room visits as well as inpatient hospitalizations was collected. Using SPSS, linear regression models were used to determine the relationship between VTE and healthcare consumption.
Results: Of the 31 patients in the study, 10 developed VTE (32%). All patients who developed a VTE were placed on therapeutic anticoagulation with 50% of patients experiencing related complications. Patients with a VTE had an increase in inpatients days (21.3 days) as compared to their non-VTE counterparts (10 days), (p=.04). There was a trend towards increased utilization of the emergency room with an average of 5.1 visits in patients with VTE as compared to those without (2.89), (p=0.244). A limited cost analysis found that anticoagulation management alone generated an additional $84,335 in healthcare costs. A full cost analysis is currently underway.
Conclusions: The development of VTE in patients with MG increases inpatient admissions days and pharmaceutical costs related to anticoagulation. While limited in patient number, this represents the first assessment of health care burden associated with VTE specific to this cancer patient population.
Skeletal Muscle Metastases Masquerading as Micro-abscesses
H. Wright, S. Kodali, F. Khan, K. Butnor
University of Vermont Medical Center
Background: Skeletal muscle metastases from lung cancer is a rare phenomenon associated with a poor prognosis. We present a patient with stage IV poorly differentiated epithelioid lung cancer who later presented with skeletal muscle metastases masquerading as micro-abscesses.
Methods: 73-year-old male diagnosed with stage IV poorly differentiated epithelioid lung cancer favoring squamous histology. Imaging showed spiculated right lower lobe lung nodule and large pleural-based masses in the right middle and lower lobes. Patient received 2 cycles of chemotherapy with carboplatin and paclitaxel. 3 months post-diagnosis, he was admitted to our hospital with right thigh pain.
Results: CT scan of right lower extremity showed edema of the right thigh musculature. MRI of right lower extremity confirmed the above findings with suspected microabscesses. He was started on antibiotics due to concern for pyomyositis. Due to worsening clinical course, biopsy of the right vastus medialis muscle was done which revealed poorly differentiated epithelioid malignancy morphologically similar to his primary lung cancer. Patient was treated with palliative radiation to his right thigh. He was readmitted within a month with intractable pain and as per his wishes, he was transitioned to comfort measures.
Conclusions: Skeletal muscle is a hostile environment for tumor cells due to high metabolic activity and blood flow variability. Thus metastases are rare. Even-though there are no guidelines on optimal management in these circumstances, palliative radiation/surgery could be employed. Our case report represents a rare manifestation of lung cancer with metastases to the skeletal muscle musculature and its associated poor prognosis.