A single institutional review of the impact of geographic location and socioeconomic status on the outcomes of adults with Acute Myeloid Leukemia
Odeth O. Barrett-Campbell1, Jonathan Pirruccello2, Raven Bennett3, Liying Pan4, Swaroopa Yerrabothala1, Frederick Lansigan1,
- Norris Cotton Cancer Center, Dartmouth-Hitchcock Medical Center, Lebanon, NH
- Department of Medicine, Dartmouth-Hitchcock Medical Center, Lebanon, NH
- Geisel School of Medicine at Dartmouth, Hanover, NH
- Guarini School of Graduate, Hanover, NH
Introduction
We conducted this study to identify if travel distance to DHMC, income, education and poverty status play a role in survival disparities, in our predominantly rural population.
Methods
Our retrospective chart review included ~180 adults with AML who received primary treatment at DHMC from 1/1/2010 - 12/31/2020. The patient’s 5 digit zip code determined travel distance to DHMC, income, poverty and education. Molecular/cytogenetic markers determined AML risk and the type of induction chemotherapy regimen documented.
Results
89 pts met criteria (64% males and 36% females). 31 patients had intermediate risk disease, 5 favorable risk, status unknown for 2. 62 patients received intensive chemo while 27 received less intensive regimen. Univariate analyses showed no effect of travel distance, income, poverty or education on remission or relapse rates. This was adjusted using gender, age and AML risk type and no correlation was seen. There was a significant difference in survival outcomes between the two treatment arms (p=0.001), with improved survival in aggressive chemo arm. Females had better chance of survival (p=0.02) and older age was a negative predictor of outcome (p=0.007).
Discussion
There was no significant difference in treatment outcomes based on travel distance to main cancer site, which may be due to the quality of care delivered at satellite sites that are part of DHMC. This also points to the need for referral to a tertiary care center even for patients receiving less/non-intensive chemo by community oncologists for consultation which will establish path for ongoing discussion and improvement of patient care.
References
Acharya U, Halpern A, Wu Q et al (2018). Impact of region of diagnosis, ethnicity, age and gender on sirvial in acute myeloid leukemia (AML). Journal of Drug Assessment. doi: 10.1080/21556660.2018.1492925
Byrne M, Halman LJ, Koniaris L et al. Effects of poverty and race on outcomes in acute myeloid leukemia. American Journal of Clinical Oncology. 2011 Jun;34(3):297-304. doi: 10.1097/COC.0b013e3181dea934.
Freeman A., Meyer A-M, Smitherman A et al (2016). Statewide geographic variation in outcomes for adults with acute myeloid leukemia in North Carolina. ACS Journals. https://doi.org/10.1002/cncr.30139
Hartmut D, Weisdorf D & Bloomfield C (2015). Acute Myeloid Leukemia. N Engl J Med 2015; 373:1136-1152. DOI: 10.1056/NEJMra1406184
Patel M, Ma Y, Mitchell B S & Rhoads KF (2012). Understanding disparities in leukemia: a national study. Cancer Causes Control. 2012 Nov; 23(11):1831-7. doi: 10.1007/s10552-012-0062-3. Epub 2012 Sep 13
Findings from the Statewide Survey of NH Cancer Survivors
Scot Foster, NH Division of Public Health Services/Chronic Disease Section, Adriane Burke, MPH NH Division of Public Health Services, Whitney Hammond, MSW, MPH, NH Division of Public Health Services
Background: The NH State Department of Health (SDOH) distributed a statewide survey of people that have been diagnosed with cancer in order to better understand their experiences.
Methods: A web-based survey was distributed to NH citizens through multiple avenues including social media, NH Cancer Centers, and other partners. The survey was completed by 588 people being treated for cancer of having completed cancer treatment. Results were tabulated and data analysis was completed by the UNH Survey Center and NH Cancer Program staff.
Results: Findings from the survey include:
- 25% (N=145) of respondents reported their mental health as fair or poor.
- 43% (N=228) of respondents reporting they exercise less than three times per week.
- 54% (N=203) of respondents that have completed treatment feel only somewhat prepared or not prepared in making the transition from actively being treated for cancer to post-treatment care.
- Survey results also collected cancer patients’ top 10 concerns, what needs they felt were unmet by their care team, where they go to for more information, and what programs or services patients feel they’d like to see more of.
Conclusions: The data indicates a need to improve access to survivorship programs that specifically target nutrition, exercise and mental health, and can also help oncology professionals better meet the needs of their patients.
This project was funded by the Centers for Disease Control and Prevention
Nursing Self-Efficacy at an Academic Medical Center
Elizabeth McGrath, DNP, AGACNP-BC, AOCNP, ACHPN, DHMC - Norris Cotton Cancer Center, Heather Blunt, MSLIS, Colleen Whatley, MSN, CNS, RNC-OB,Ian Kirit, MSN, RN, CEN
Affiliation: Dartmouth-Hitchcock
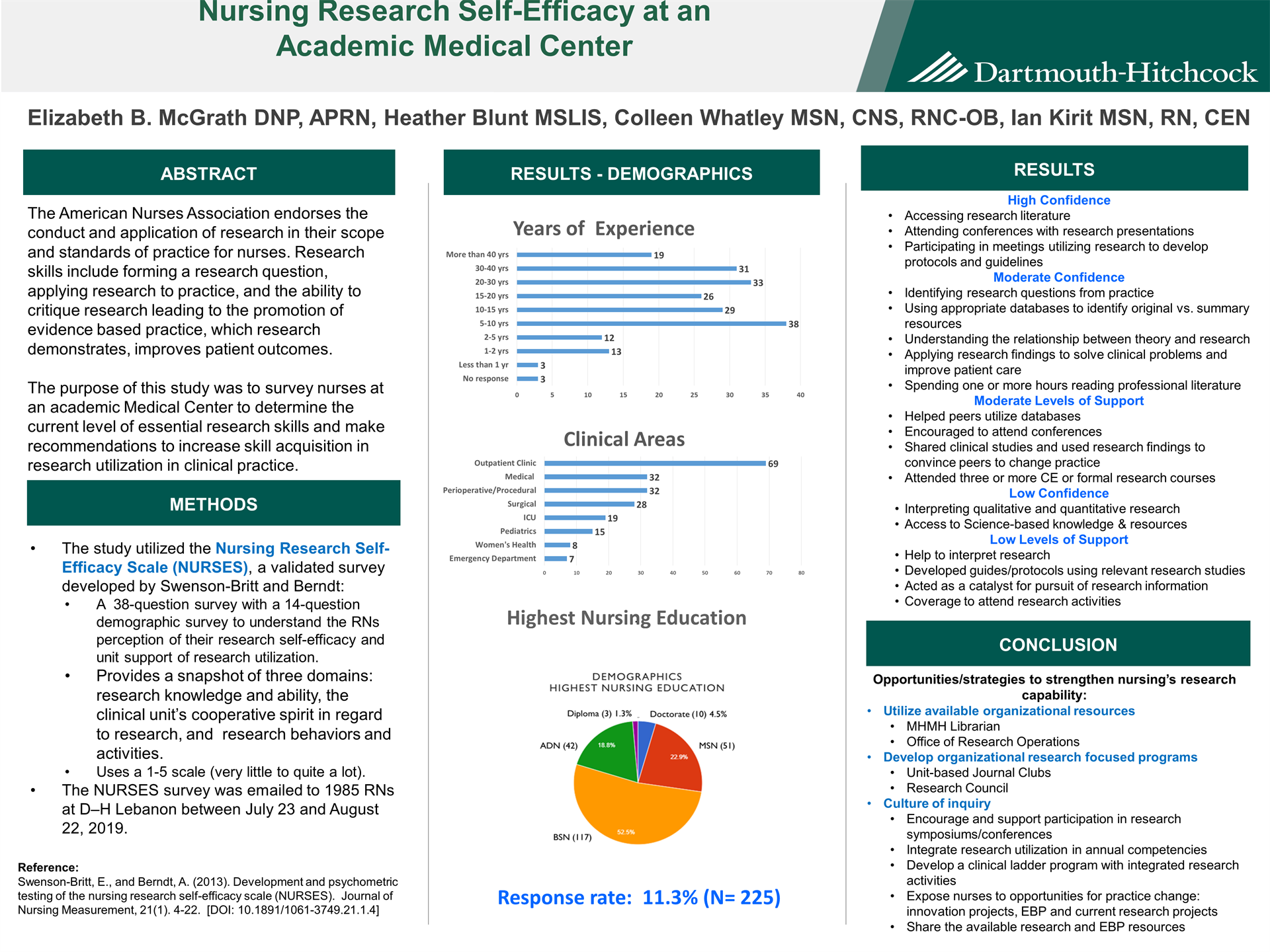
Background: The American Nurses Association endorses the conduct and application of research in their scope and standards of practice for nurses. Research skills include forming a research question, applying research to practice, and the ability to critique research. The purpose of this study was to survey nurses at an academic Medical Center to determine needs related to research and evidence-based practice.
Methods: The study utilized the Nursing Research Self-Efficacy Scale (NURSES) developed by Swenson-Britt which utilizes a 38-question survey with a 14-question demographic survey to better understand the RNs perception of their research knowledge and ability, the clinical units cooperative spirit in regard to research, research behaviors and activities, and general demographic information. The survey was emailed to 1985 RNs at D–H Lebanon between July 23 and August 22, 2019.
Results: Response rate was 11.3% (N= 225). Respondent's clinical experience ranged from 6 months to < 40 years with 13 years as both the average and median years of clinical experience. The majority of nurses were from inpatient settings followed by ambulatory, perioperative and emergency medicine. Respondent’s highest level of education were BSN (52.5%), followed by MSN (22.9%) and ADN 18.8%. 50% reported high confidence how to access research literature through Internet search engines, attendance at conferences where research is presented, and participation in meetings that utilized research to develop or influence protocols, guidelines, process improvement. Moderate cooperative spirit was identified in the embedded clinical units.
Conclusions: Several areas were identified in need of more support which will be presented with recommendations.
On-site Rural Cancer Center Fresh Food Pantry to Feed Body, Mind and Soul
Catherine M Reed MSW, LICSW1, Chelsey R Canavan MSPH2, Greg A Norman MS2, Jeannine B Mills MS, RD, CSO, LD1, Lisa Champagne CHW1, Elizabeth B McGrath DNP, APRN, AGACNP-BC, AOCNP, ACHPN1, John M Hill Jr MD1 and Kenneth R Meehan MD1
1Department of Hematology/Oncology, Norris Cotton Cancer Center, Dartmouth-Hitchcock Medical Center, Lebanon NH
2Department of Population Health, Dartmouth-Hitchcock Medical Center, Lebanon NH
Background: At our rural cancer center we routinely help patients with hospital financial assistance, private foundation grants, and transportation. However, until inquiring specifically about dietary intake, we were missing an epidemic of food scarcity hidden in plain sight. One patient was eating only peanut butter, crackers, and risotto in preparation for a complicated and costly stem cell transplant.
Methods: We asked our patients specifically about food insecurity and instituted social determinants of health screening with validated Hunger Vital Signs questions. An EPIC Best Practice Alert notified the care team in real-time of patients needing food. A local community food pantry delivered fresh produce, dairy and staples to our pantry. A social worker took orders, packed bags, and delivered food directly to patients’ cars.
Results: In the first six weeks we provided 35 food-insecure patients with two weeks of healthy food for their households. This included four stage IV GI/Oncology patients and several cellular immunotherapy recipients. Nutrition was given to support chemotherapy, radiation, surgery and transplant tolerance, and patients volunteered feeling less anxious and more hopeful. One stated, “It helps so much when one is down and out and things are falling down around you. This is amazing!” Biopsychosocial disclosures also notably increased.
Conclusions: An on-site, rural cancer center food pantry benefits food-insecure patients who are exhausted, nutritionally at risk and financially compromised, especially during a pandemic. Fresh food should be considered vital, up-front cancer treatment and part of a holistic effort to treat the whole person in this devastating predicament.
.png)